CPT 99483 is a valuable code for billing time spent assessing and planning care for patients with cognitive impairment, such as Alzheimer’s disease or other forms of dementia. However, because CPT 99483 requires caregiver involvement, providers should switch to an appropriate E/M code when no caregiver is available.
Understanding CPT 99483 and Its Requirements
CPT 99483 is a code used for care plan oversight in patients with cognitive impairment. This service includes activities such as:
- Assessing and developing a comprehensive care plan
- Reviewing the patient’s cognitive and functional status
- Coordinating care and providing education for both the patient and their caregiver
- Recommending interventions for managing cognitive decline
A key requirement for billing CPT 99483 is the involvement of a caregiver in the patient’s care plan. The caregiver plays a crucial role in the patient’s daily routines, monitoring symptoms, and assisting with care, which is why this code is designed for situations where a caregiver can be actively involved in the process.
Billing cognitive assessment without a caregiver
When a patient has no caregiver—whether due to living alone, family absence, or other reasons—the requirements for CPT 99483 cannot be fully met. The absence of a caregiver means there is no one available to provide support for the patient, which is essential to the care coordination component of this code.
Alternatives to CPT 99483
If a caregiver is not available, you’ll need to consider an appropriate Evaluation & Management (E&M) code instead. E&M codes are used to bill for patient visits where the focus is on evaluating the patient’s condition and providing management services. These codes do not require the involvement of a caregiver.
Depending on the complexity of the patient’s condition and the extent of the visit, you may bill for one of the following E&M codes:
- CPT 99202-99215: These codes correspond to office or other outpatient visits, ranging from simple to high complexity visits, depending on the level of decision-making and time spent.
- For example, if you spend a significant amount of time with the patient evaluating their cognitive function and providing recommendations, a higher-level E&M code (e.g., 99214 or 99215) may be appropriate.
Key Points for Billing Without a Caregiver
When switching from CPT 99483 to an E&M code, be sure to consider the following:
- Time and Complexity: The E&M code you select should reflect the time spent and the complexity of the assessment. If you are spending more time on cognitive evaluations or managing a complex case, you should bill for a higher-level E&M code.
- Documentation: Accurate and thorough documentation is crucial. Ensure that you document the patient’s cognitive status, functional abilities, and any interventions or treatment recommendations you discussed. You’ll also want to record the fact that there was no caregiver available to participate in the care plan.
- Care Plan Review: Even without a caregiver, you can still create and review a care plan with the patient. This could include recommendations for future cognitive assessments, referrals to specialists, and non-pharmacological interventions (e.g., memory aids, structured routines). Be sure to document these discussions thoroughly.
- Patient Education: Provide education on cognitive impairment and offer resources for the patient to follow up on (e.g., support groups, community services). These discussions help justify the need for a higher-level E&M code.
Conclusion
CPT 99483 is a valuable tool for billing cognitive assessments when a caregiver is involved. However, in situations where a caregiver is not available, it’s important to switch to the appropriate E&M code to reflect the time and complexity of the visit. By accurately documenting the patient’s condition, the complexity of the visit, and any interventions provided, you can ensure that the billing reflects the services delivered and that you’re appropriately reimbursed for your efforts.
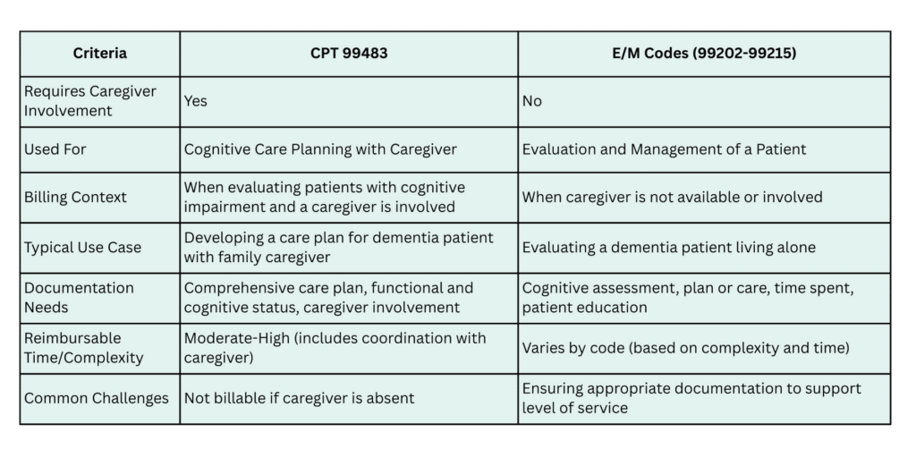
Comparison between 99483 and E/M Codes 99202-99215